Oh no! You got lost on the moose trail!
The page you are looking for no longer exists. But don't hurry off! Stay awhile & look around! Turn this into a happy little accident and find your new favorite blog post!

Let's chat about natural, holistic, & happy living while making it super simple & fun!
Join The Crunchy Moose community and I'll send you a free copy of my eBook The Beauty Remix full of your new favorite DIY recipes!
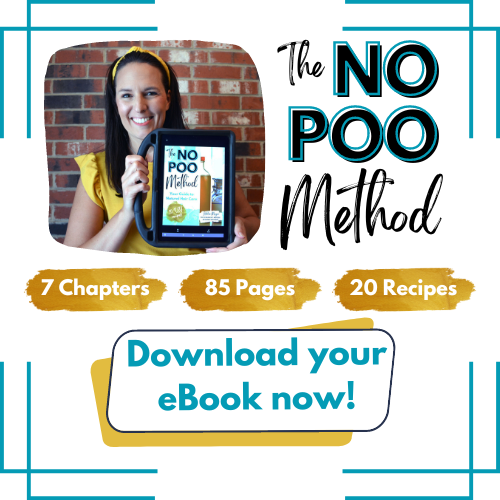
The No Poo Method eBook
The No Poo Method is your guide to find a natural hair care routine that works for you, at whatever level you want to take it.
Are you ready to dive right in and ditch all your commercial hair products? This book will walk you through that process!
Or do you just want to learn how to naturally nourish your hair with an occasional deep conditioner or serum That’s here, too!